-
Credits
- Story by:
- Aleksandra Sagan & Laura Kane
- Edited by:
- Sunny Freeman & Kevin Ward
- Layout & Graphics by:
- Lucas Timmons
- Graphics by:
- Sean Vokey
- Produced by:
- Megan Leach

ESHOWE, SOUTH AFRICA — Catherine Booth Hospital in rural South Africa perches atop a long, winding road, overlooking lush, green fields. Ambulances drive along the bumpy path carrying emaciated people from the cities and villages scattered nearby to spend months — if not years — enduring toxic treatment for an infectious, airborne superbug.
Drug-resistant TB wreaks havoc on the body. Infected people cough so violently they spit up blood and pieces of their lung lining. Their chest aches and fever spikes. Their body weight plummets and they transform into a skeletal frame.
On a blistering hot day, one man slowly shuffles his body toward a wheelchair. He wears only a diaper beneath an open robe, and his skin stretches taut over his bones. His knees are easily the widest part of his legs.
“My first thought was that I’m going to die ... I’m really going to die,”
Drug-resistant tuberculosis survivor Tsholofelo Nombulelo Msimango
Drug-resistant tuberculosis is the world's deadliest superbug. It develops when bacteria that causes tuberculosis, a disease believed to be as old as mankind, stops responding to drugs used to treat it, largely because health-care workers improperly prescribe medicine or patients stop treatment early. Infected people can spread it through the air when they cough.
Often, a victim's only fault is breathing.
It took Tsholofelo Nombulelo Msimango a long time to realize she wasn't to blame when she caught the infectious disease at 19 years old.
When it came, it stopped her entire life. Doctors told her she must stay in hospital, swallow more than a dozen pills daily and receive painful injections five days a week for six months if she wanted to live.
"My first thought was that I'm going to die ... I'm really going to die," the now 24-year-old recalls from her home in a township near Johannesburg.
Health-care workers diagnose hundreds of thousands of people with drug-resistant TB each year. By 2050, the disease is expected to account for about one-quarter of a projected 10 million annual deaths from all drug-resistant infections around the world.
Four drugs make up the first-line of defense against tuberculosis. If a patient's strain is immune to at least two of these, it is considered multi-drug resistant (MDR-TB). If it's unresponsive to most of the drugs doctors turn to next, the diagnosis escalates to extensively-drug-resistant TB (XDR-TB).
An estimated 600,000 people developed or required treatment for multi-drug-resistant TB in 2016, according to the World Health Organization's most recent annual report on the disease.
South Africa is burdened with some of the highest numbers of tuberculosis and drug-resistant TB cases in the world, the WHO says. More than 20,000 laboratory-confirmed cases required MDR- or XDR-TB treatment in 2016.

While the infectious disease remains rare in Canada, travellers to and from the country give bacteria ample opportunity to hitch a ride and spark an outbreak.
People carrying multi- or extensively-drug resistant TB can spread it to others by coughing. Sharing a bedroom, bus or break room with closed windows can result in transmission.
In countries with elevated levels of infection, health-care providers struggle to contain the disease that slowly ravages the body.
They work against poverty and stigma, with inadequate diagnostic tools and long, toxic treatment regimens that prompt many patients to stop before they're cured, while remaining infectious to others.
Patients put their lives on pause for months, sometimes years, for treatment. Depending on severity, the odyssey can include a hospital stay of more than a year, dozens of pills daily and a painful injection into the buttocks each day for six months.
Workers at Cape Town's Brooklyn Chest Hospital recall knowing exactly when nurses inject patients with medicine because the screams emanating from another building interrupt their staff meetings. Some patients describe it as lava — a fire-like sensation washing over their body from where the needle enters.
The list of side effects seems never ending. Some patients permanently lose their hearing, experience psychosis or feel constant nausea. Their kidneys can fail, their hands and feet can sting with pins-and-needles sensations, and their skin can change colour.
"It was hell," says Nombulelo Msimango of her two-year treatment plan. "I felt like my life was over."
After seven months, Nombulelo Msimango secretly decided to stop treatment. She hid the pills from her family.
It's a common reaction, say health-care workers, some of whom recount regularly finding medicine tossed over hospital walls or empty beds after patients escaped overnight.
"It used to happen all the time," says Julian te Riele, a family physician at Brooklyn Chest Hospital who oversees the adult male XDR-TB ward.
“It was hell. I felt like my life was over.”
Drug-resistant tuberculosis survivor Tsholofelo Nombulelo Misimango
"There were pills in the dustbins, pills outside the windows, pills everywhere," he says, adding that's become less of a problem as doctors gained access to some newer drugs, like bedaquiline, to replace those that give patients unbearable side effects.
Disrupted treatment feeds into the vicious cycle of drug resistance. The bacteria grow stronger and medicines that previously worked no longer do, leaving doctors with fewer — if any — treatment options.
"It takes a lot longer to kill those sleeping bugs. And, if you don't take your pills, they wake up later and they wake up stronger," says te Riele.
About a month after Nombulelo Msimango stopped treatment, her health deteriorated. She coughed up blood and saw an emaciated face in her mirror. She landed in a hospital and stayed for a year.
Her TB upgraded to XDR, possibly because she interrupted treatment, or possibly because of an initial misdiagnosis. Either way, she cried for most of that day.
Until recently, patients faced a harsh choice: cure TB, but lose their hearing, or stop treatment and let the TB kill them. Now, with the arrival of some new drugs, doctors perform tests on patients and try to switch them to a different medicine as soon as they show any signs of hearing loss.
The prospect of life in silence terrified musician Lizahn Kemp, who at 25 years old was shocked to learn the lymph nodes swelling on her neck stemmed from MDR-TB.
"Music is my life," she says. "I can deal with other stuff, but I can't deal with not hearing."
So much so, she attended a music festival for several days rather than admit herself to hospital immediately, as her doctor ordered in April 2016. It was only when she woke up at the festival with one of her lymph nodes oozing that she realized the seriousness of her illness.
Several months into receiving the injectable she noticed trouble with her hearing — a fear a medical test quickly confirmed. She immediately swapped the medicine out of her daily regimen, but she says she'll never regain the small percentage of hearing she lost in one ear.
"The ringing, I can always hear."
Physical side effects, as Kemp knows, are only half the story.
The medication made the artist feel emotionless and half-dead inside. She no longer wrote short stories or music lyrics.
"It's literally feeling like you're in a prison," she says.
Sometimes in those dark moments, patients' thoughts can turn to suicide.
After Sipho Luthuli learned he had MDR-TB, the 20-year-old sometimes contemplated killing himself.
“It’s literally feeling like you’re in a prison,”
DR-TB survivor Lizahn Kemp
He spent a lonely month at Catherine Booth Hospital, far from the compound where he lives with his extended family in rural Eshowe. They only visited him once in 28 days because of financial constraints, he says in isiZulu through a translator.
Luthuli left school halfway through grade 11 to fight the disease. Instead of working towards graduation, the teenager, who believed a diploma would be the ticket to better his family's circumstances, felt isolated from his former schoolmates and spent his days taking medicine. Its smell alone made him nauseous.
He feared the daily injections, intermittently lost his hearing and developed a rash.
When the side effects, treatment and alienation became too much, Luthuli wondered if he'd rather just die.
Listen to Lionel's mom talk about how the playful boy's personality changed when he got sick.
Lionel Flores missed his mom Gladys Najoe while she was in a hospital treating her tuberculosis. He stopped playing, eating and communicating. He started vomiting and soiling his bed at night. But it turned out those were symptoms. He had multi-drug resistant tuberculosis meningitis, which lives in the brain.
When he arrived at Brooklyn Chest Hospital last November, he couldn’t move any of his limbs, but his right arm. He couldn’t speak, and though he could recognize his mother, couldn’t say, “Mama.”
His mom and aunt worried he’d never be able to walk or talk again. It made them sad to think of how he used to run and play ball.
Thanks to a daily cocktail of medicine that doctors crush and put in a drink for him, Lionel eventually started to talk, eat and sit up. A few months later, he could walk around by himself, slightly dragging one leg.
He’ll likely have to stay on treatment for at least a year, and it’s unclear when his mom will be able to take him home - much of that rests with when she starts to feel better.
Despite such difficulties, it's crucial patients start and stay on the right medication to save their lives and prevent them from infecting others. Yet, until recently, doctors needed weeks to diagnose resistance, sometimes starting patients on possibly ineffective medication that could further fuel the problem.
Health-care workers detect only one in four MDR-TB cases, the WHO estimated in a 2015 report, and cure only half.
In recent years, a new test for a platform called GeneXpert emerged to address that problem. It allows doctors to diagnose TB and check for resistance to one of the four front-line TB drugs in a matter of hours, providing a good indicator for an MDR-TB diagnosis.
"That was really a game changer," says Heidi Albert, head of the Foundation for Innovative New Diagnostics in South Africa.
But the platform requires infrastructure that may not be present in rural communities and cannot test for resistance to a wider range of medicine.
TB patients also face stigma and many showing symptoms may avoid seeking help.
People still tend to believe patients with drug-resistant TB can't be cured and remain incredibly contagious, even after treatment begins.
Stories abound of young women unable to marry after a TB diagnosis, communities forcibly expelling infected individuals, and friends and family alienating patients. Even health-care workers may shun their charges with drug-resistant TB, fearing they'll catch the disease.
Xoliswa Harmans remembers the day she heard her XDR-TB diagnosis; a nurse at the clinic forced her to wait outside the gate for an ambulance to the hospital.
"I was just like a ghost," she says.
Poverty also plays a role in the spread of TB, especially in informal settlements known as townships and remote areas. Multiple generations typically share one or two rooms in cramped, makeshift houses in the townships. They are relics of the country's apartheid history, a visual reminder that segregation persists.
Patients from such communities may not be able to afford the couple of Canadian dollars it would cost to travel to a clinic to pick up medicine or undergo testing, or to stay in a hospital and forego work.
They may share a windowless bedroom with multiple family members, putting their family at higher risk of infection. They may struggle with drug or alcohol addiction, making them less likely to stick to a treatment plan, or lack education and believe that traditional healers, who provide herbs and other remedies, will cure them.
Listen to Gervinho's mom explain her fears about whether her son will fully recover.
Gervinho Swart developed a fever and lost his appetite before his second birthday. His parents, Carmelita and Gerrit Swart, took him to the hospital where he had what his mom describes as an almost stroke-like fit. Doctors conducted tests and discovered Gervinho has multi-drug-resistant tuberculosis meningitis.
He lives at Brooklyn Chest Hospital in a ward with several other toddlers. He must swallow multiple pills daily and receive a painful injection that’s turned his bum blue and purple. When his mom asks him where it hurts, Gervinho shows her his bottom.
His parents are able to take him home on the weekends and spend that time going to the park and eating ice-cream. But Carmelita says the hardest part is returning home empty handed after dropping him off at the hospital for his weekday treatment and seeing all his things - like clothes in the wash - at home.
Still, she’s thrilled her first and only child is regaining his strength. He went from looking “like a zombie,” Gerrit says, to walking and playing like most other children his age.
His treatment will last more than a year, but Carmelita and Gerrit are hopeful they’ll be able to bring him home for good soon.
While eastern Europe, Asia and Africa bear the brunt of the disease's burden, living in Canada doesn't provide immunity because bacteria do not respect borders.
In 2017, more than 1.2 million people from the 20 countries the WHO identifies as having the highest MDR-TB burden in the world, including South Africa, visited Canada, according to Statistics Canada.
In 2016, Canadians travelled to those 19 of those 20 countries more than 1.6 million times. The agency did not provide data for North Korea.
Up until the end of April 2018, Canada admitted nearly 63,000 permanent residents from these countries, according to data compiled by Immigration, Refugees and Citizenship Canada.
Angeline Doonan moved to Vancouver from South Africa in August 2014. She fell ill a few months later, despite passing all the necessary health checks before her departure.
By that fall, she was experiencing coughing fits and fractured a rib from one particularly bad bout. A doctor at a walk-in clinic believed she had a chest infection, but sent her for an X-ray just in case.
Tests revealed Doonan's diagnosis: multi-drug resistant tuberculosis. She spent the first several months of 2015 in a negative pressure isolation unit at Vancouver General Hospital.
Doonan describes the beginning of her illness as a blur, as doctors "slammed" her body with different medications.
Her weight plummeted to about 95 pounds and her muscles atrophied, nearly all the nails on her fingers and toes fell off, her skin turned purple and she developed neuropathy — a sensation that felt like every pore was on fire that left her itchy and twitching.
"It was really hard looking in the mirror and seeing somebody that you don't recognize," she says.
After five months in the hospital, Doonan continued treatment until her nearly two-year journey ended in September 2016, when doctors finally uttered the word she longed to hear: cured.
She goes for follow-up visits every six months and contends with some long-term effects, like continued neuropathy and gastrointestinal issues.
While in hospital, Doonan says the rooms in her unit dedicated to TB patients were mostly full.
Listen to Owam's mom explain why her daughter needs to live in the hospital.
Owam Sisilana’s mom, 24-year old Siyamthanda Sisilana was undergoing treatment for multi-drug-resistant tuberculosis when they noticed the little girl was losing weight. She took her daughter to the doctor and tests showed she had acquired the multi-drug-resistant infection.
She sleeps in a sparsely decorated, double room in the children’s ward at Brooklyn Chest Hospital. During the day, Owam plays with other kids. But that distraction disappears at night when she’s in bed, crying and missing the three family members she shares a room with back home.
As long as Owam is contagious, she won’t be allowed back home for a weekend visit. Her mom and grandmother take turns visiting, so she’s not alone for more than a one-day stretch.
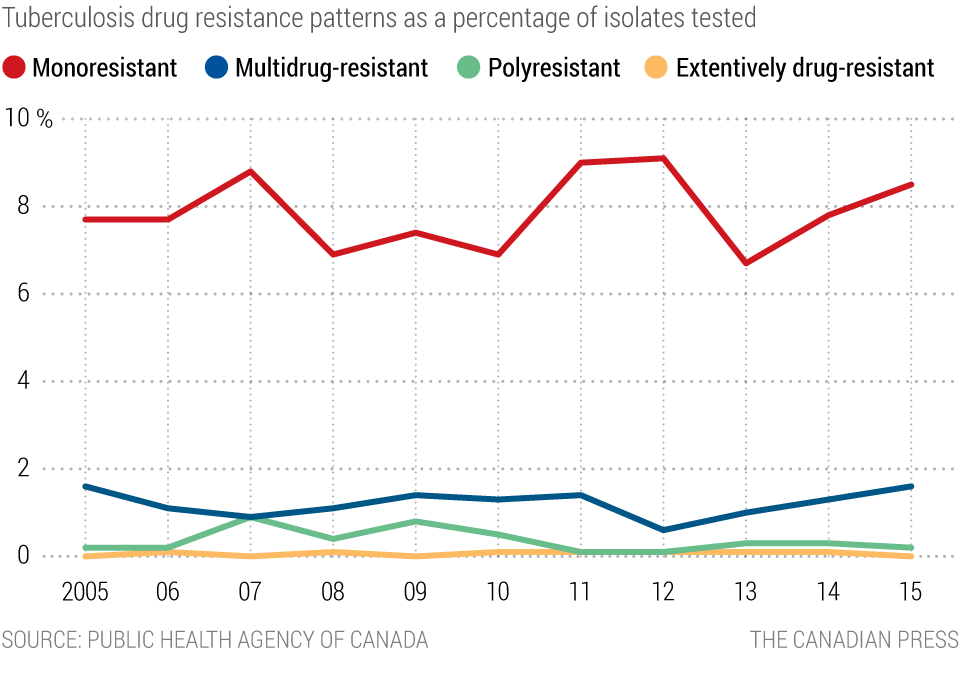
Between 2006 and 2016, 173 samples tested in Canada were classified as MDR-TB and seven as XDR-TB, according to a government report on drug resistance. A majority of tuberculosis cases occur among people born outside of Canada, like Doonan, according to government data.
The federal government is in discussions with the provinces and territories to expand testing for new arrivals to include scans for latent TB, in which people infected with TB bacteria do not show signs of active TB and are not contagious, but can develop it later. It did not provide a timeline for implementation.
While both travellers returning to Canada and newcomers may bring a drug-resistant strain into the country and infect others, there is one Canadian community of particular concern to experts: the Inuit.
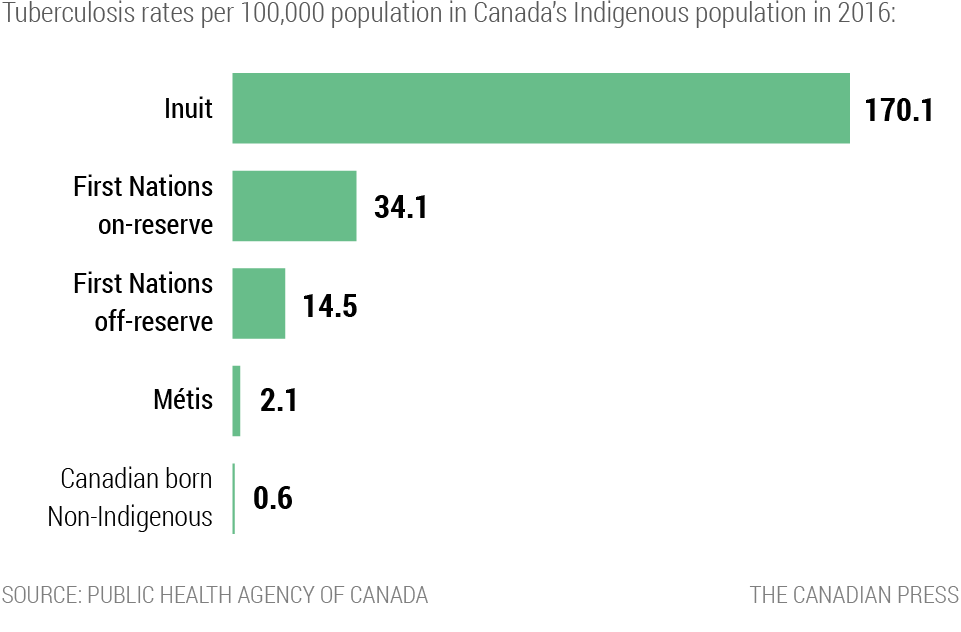
In 2016, Inuit people experienced TB at a rate of 170.1 per 100,000, according to government data, nearly 300 times higher than the rate for people born in Canada who are not Indigenous.
It's unclear why drug-resistant TB has not developed and thrived in Inuit Nunangat, the four Inuit regions in Canada where almost three quarters of the nation's roughly 65,000 Inuit population lives. Some attribute it to Canada's advanced health-care system, while others suggest the disease is more prone to spread in tropical areas.
“I’m inclined to think at this point that we have been lucky to avoid it.”
Pediatric diseases specialist Ashley Roberts
But the community appears primed for an outbreak. Colonization left behind long-term consequences including poor living conditions, with overcrowded houses that need repairs and lack good ventilation; unreliable access to food leaving some hungry and malnourished; and problems accessing health care because of distance, language or other barriers.
The combination allows for more effective transmission, says Ashley Roberts, a pediatric diseases specialist at BC Children's Hospital in Vancouver.
"I'm inclined to think at this point that we have been lucky to avoid it."
On this year's world TB day in March, Indigenous and Northern Affairs Canada called the high TB rates among the Inuit a "staggering and unacceptable reality." It promised to eliminate TB cases in Inuit Nunangat by 2030.
The milestone, if reached, would land several years ahead of the WHO's global plan to reduce TB cases by 90 per cent globally by 2035, including drug-resistant TB.
Some progress has been made. GeneXpert helped better diagnostic capabilities and successful drug trials allowed doctors to shave a few months and pills from standard treatment regimens.
But all that's been done is still a far cry from the investment into research and resources that experts say is needed to combat the growing epidemic.
Health-care workers need better diagnostic tools to identify resistance quickly and accurately. Patients need shorter, less harmful drug regimens so they finish treatment. Those changes are necessary, experts say, to tackle not only drug-resistant TB, but all superbugs.