-
Credits
- Story by:
- Laura Kane & Aleksandra Sagan
- Edited by:
- Sunny Freeman & Kevin Ward
- Layout & Graphics by:
- Lucas Timmons
- Produced by:
- Megan Leach

NEW DELHI — Vikali A Zhimomi's face is tear-streaked as she reaches out to touch her infant grandson, who is receiving intravenous fluids after emergency surgery. She is forbidden from picking him up, as desperately as she wants to. His tiny body is simply too fragile.
The little boy developed severe diarrhea just days into his life. A Zhimomi rushed him to a hospital in northeast India, where doctors discovered necrosis in his bowels and removed part of his small intestine. But a bacterial infection soon spread into his bloodstream and antibiotics were not working.
The panicked grandmother took the child and boarded an air ambulance to Sir Ganga Ram Hospital, a private New Delhi facility, where another surgery was performed. Doctors placed the four-week-old on colistin, a last-resort antibiotic and the only drug left that might cure his otherwise resistant infection.
"Every day I pray to God," says A Zhimomi, her eyes bloodshot with exhaustion.
"I've been touching his abdomen every day. I pray for the doctors every day."
Listen to Vikali A Zhimomi talk about the impact that her grandson Atomika had on her life.
She is terrified — and with good reason.
A 2013 study estimated 60,000 infants in India die annually from sepsis caused by antimicrobial-resistant infections, and the expert who calculated the figure now believes the rate to be double that.
Doctors increasingly treating babies with colistin see even those just born carry a frightening resistance to the drug. They worry about what to do when that last line of defence fails.
The situation is desperate and not confined to developing countries.
In Canada, hospitals also grapple with the rise of dangerous superbugs. The rapid spread of a highly resistant enzyme from South Asia to the West illustrates the global nature of drug resistance.
Families of victims are calling on global leaders to pay attention and curb the rampant overuse of antibiotics that accelerated the crisis.
A Zhimomi is raising her grandson after his teenage mother, who had a relationship with A Zhimomi's young son, decided she could not care for the child. The 43-year-old is a community leader in Dimapur, in the northeastern state of Nagaland, where she ran for political office and founded a women's empowerment group.
She has high hopes for the grandson she named Atomika, meaning a leader among leaders.
"They said, 'Do anything to save the baby.' "
Chairwoman of the neonatology department at Sir Ganga Ram Hospital Dr. Neelam Kler
"The moment I saw his face, I stopped calling my friends. ... I felt that this is my life," she says. "A big happiness has come inside of me. … I am focusing on him only."
Colistin eventually eradicated the little boy's infection and he was discharged from hospital, where staff are also grateful for his survival.
Listen to neonatologist Dr. Neelam Kler talk about the risks of drug-resistant infections in premature babies.
"We never thought he would make it," said Dr. Neelam Kler, chairwoman of the neonatology department at Sir Ganga Ram Hospital, adding the family consented to a very high-risk surgery.
"They said, 'Do anything to save the baby.' "
In India, 26 million babies are born every year. Of those, Kler says roughly 650,000 die in infancy, and about 25 per cent of those deaths are caused by infection.
"If I see a 500-gram baby or a 28-week baby, my biggest concern is that this baby should not get an infection because he's the most vulnerable," Kler says.
"If he gets an infection, and it's multi-drug resistant, then I'm doomed, totally."
Over her 30-year career, Kler has observed a dramatic rise in bacterial infections resistant to numerous antibiotics. Organisms such as E. coli and Klebsiella evolved to fight off more powerful drugs, to the point that many cases Kler sees are resistant to meropenem, a broad-spectrum antibiotic once reserved for severe instances.
There are many reasons for the growth of antimicrobial resistance, but Kler is particularly concerned about three issues in India: pharmacies sell antibiotics without a prescription; crowded hospitals lack strong infection control; and few diagnostics are available to confirm bacterial infections before antibiotics are started.
"It is depressing. It is alarming," Kler says.
"If he gets an infection, and it's multi-drug resistant, then I'm doomed, totally."
Chairwoman of the neonatology department at Sir Ganga Ram Hospital Dr. Neelam Kler
"I think there is a need for action."
While A Zhimomi's grandson received care in a private hospital, millions of Indians rely on government hospitals that are free but overcrowded.
At Chacha Nehru Bal Chikitsalaya children's hospital, the number of patients often exceeds its 221 beds. In the summer, when infectious diseases are particularly acute, up to 270 children are admitted.
"We have to double them up," says Dr. Anup Mohta, a pediatric surgeon and director of the hospital.
"We do want one patient, one bed (but) the government policy as of now is to not refuse any patient."
The crowding leads to obvious challenges with infection control, but hospital staff do everything they can to prevent the spread of resistant bacteria. There is no doubling up on beds in the intensive care units and babies and children are sent home as soon as possible to reduce the risk of infection.
Anu and Pawan Bhalla credit the children's hospital with saving their son, Naksh.
The couple tried for a decade to conceive before Anu became pregnant with twins last year. At just six months, she delivered two boys in August, each weighing less than a kilogram. After about 10 days at a different hospital, the struggling twins were transferred to the children's hospital.
One twin died within 24 hours. But Naksh, weighing only 540 grams, continued to fight. He had every conceivable complication that comes with being born premature — jaundice, respiratory troubles, eye problems — along with bloodstream infections of Klebsiella and acinobacter. His blood culture showed he was a candidate for colistin and doctors started him on the drug.
"I was quite upset," says Anu, through a Hindi translator. "But I had faith in the doctors that my baby will survive."
The mother arrived at the hospital at 5 a.m. every day and stayed with the baby until midnight, when she and her husband returned home for mostly sleepless hours.
When Naksh was finally discharged after two months, Anu took him home for the first time. She still couldn't sleep. Instead, she stayed up all night looking at her child, healthy and safe at last.
The doctors and nurses were thrilled to discharge the baby, the lowest-weight premature infant ever saved by the hospital.
Dr. Mamta Jajoo, an associate professor of pediatrics, remembers when drug resistance became a grave concern for the hospital. It was 2008, when a Klebsiella outbreak spread to seven patients.
“If we don't even have colistin to use, then what will we do?"
Associate professor of pediatrics Dr. Mamta Jajoo
The infection could not be cured by any antibiotic in the usual repertoire. Doctors had not used colistin in decades because it has potentially severe neurological side effects, but it was the only option left. Five of the seven patients survived.
"It was because of colistin only that they were able to come out of that infection," says Jajoo.
Multi-drug resistant infections have since risen drastically and prescribing colistin has become relatively commonplace. Doctors must use it because it's the only way to save dying babies, Jajoo says.
But she's seen about two or three cases of colistin resistance in the past year.
"We are afraid," she says.
"If we don't even have colistin to use, then what will we do?"
Colistin has become the answer to increasing resistance to carbapenems, important antibiotics used to treat serious bacterial infections. Carbapenem resistance was unheard of as recently as the late 1990s. It has now become widespread in South Asia, says Ramanan Laxminarayan, director of the Center for Disease Dynamics, Economics and Policy and a leading expert.
"People say colistin is last resort. Colistin is like swallowing a poison pill to get rid of the bugs," he says.
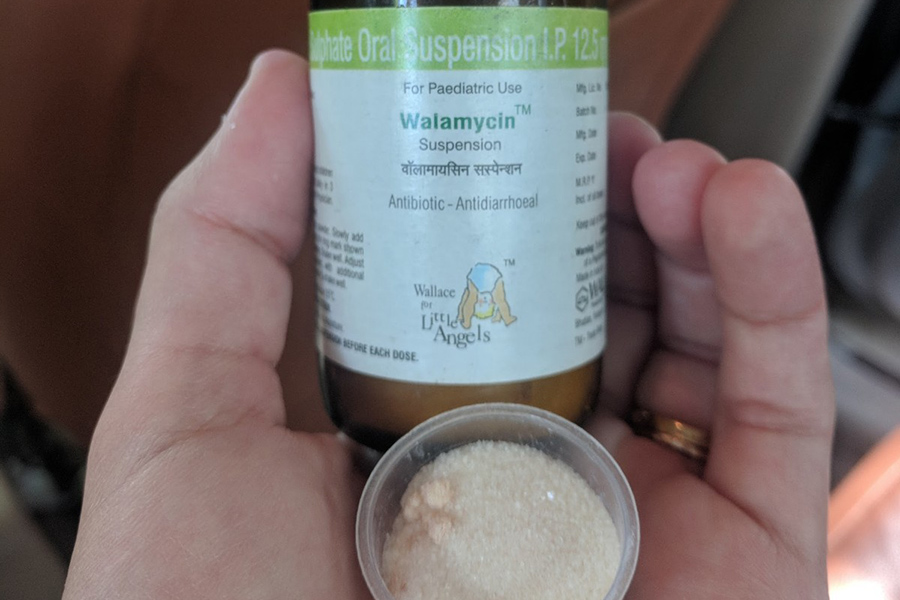
Across the street from one of New Delhi's largest hospitals, an open-air pharmaceutical market sells antibiotics over the counter. Only one shop has a sign that says antibiotics are not sold without a prescription.

Colourful chemist shops line the busy road, nestled among pungent street food vendors and aggressive postcard hawkers. Anyone can buy pediatric colistin for about C$1.25 without a prescription, though some shops don't stock the drug.
"People say colistin is last resort. Colistin is like swallowing a poison pill to get rid of the bugs."
Director of the Center for Disease Dynamics, Economics and Policy Ramanan Laxminarayan
Some argue that Indians need to be able to buy antibiotics without a prescription because of poor access to qualified doctors, particularly in rural and impoverished areas.
Experts suggest that — at the very least — people should not be able to buy crucial last-resort antibiotics over the counter. The government tried to tackle the issue with a "red line" campaign, in which more advanced drugs are marked with a red line that means a doctor's prescription is required.
But Laxminarayan calls the campaign hopeless.
"I get invited around the world to speak on the red line campaign, and I have to politely say, 'Um, there is no red line campaign,' " he says.
"They may have got the red line on a few things, but you can get red line antibiotics."
Laxminarayan authored a widely cited 2013 study that estimated nearly 60,000 newborns die of sepsis from antimicrobial-resistant infections annually in India. After reading the findings of a separate 2016 study, which observed newborns for about three years in three large hospitals in Delhi, Laxminarayan now believes about 120,000 babies die every year from sepsis caused by drug resistance.
Dr. Sushma Nangia, head of the neonatology department at Kalawati Saran Children's Hospital in New Delhi says doctors at the hospital once liberally used antibiotics in babies they suspected had a bacterial infection, even before laboratory testing.
"They may have got the red line on a few things, but you can get red line antibiotics."
Director of the Center for Disease Dynamics, Economics and Policy Ramanan Laxminarayan
Nangia now acts as the gatekeeper for all new antibiotic use.
Her residents must obtain laboratory confirmation and get her approval before starting an infant on antibiotics. A white board outside the neonatal intensive care unit tallies how many babies are on the drugs.
Inside the unit, nurses wearing blue hairnets and shoe coverings care for mostly premature babies, some as small as a hand and whose tiny ribcages rise and fall with each laboured breath.
The government hospital implemented a unique strategy to deal with crowding. It admits mothers along with their babies because breast milk is believed to be crucial in preventing and fighting infections.
---,---,---
Click the button to begin
BeginSources: Dr. Neelam Kler & Ramanan Laxminarayan
Once a baby is healthy enough, he is moved from the intensive care unit to an area where mothers sit on couches with their infants on their chests. Kangaroo-mother care, as it's called, helps keep the infant warm and promotes breastfeeding.
But having multiple mothers and babies on one couch poses infection control challenges. When the couch room becomes too full, relatively stable mothers and infants move to a unit where there are extra beds.
Sweta Saurbh, a 27-year-old first-time mother, sits on one of the beds in a room with several other moms and their babies. Her premature son lies next to her, one side of his skull swollen with a hematoma, a collection of clotted blood.
Before she gave birth, Saurbh was in hospital for a month and received intravenous antibiotics for a drug-resistant urinary tract infection. Forceps used during childbirth caused her son's hematoma, which is now colonized with the same bacteria she had.
"I thought when I saw the baby that it is because of my mistake this has happened," says Saurbh, speaking through a Hindi translator.
"I'm getting now it is not because of that. It's because of the instrument they used."
The baby's head initially swelled on both sides, but a surgical procedure successfully reduced the hematoma on one side. He is receiving colistin to treat the infection and the swelling on the other side is subsiding.
"I'm seeing so many mothers with babies going home," she says from the hospital bed a month after giving birth. "Going home means the baby is all right."
The crisis is not only unfolding in India or other parts of the developing world.
Bloodstream infections of methicillin-resistant staphylococcus aureus, or MRSA, are rising in Canadian pediatric hospitals, causing fever, chills and sometimes death.
A dangerous carbapenem-resistant enzyme called New Delhi metallo-beta-lactamase, first identified in 2008 in a Swedish patient who had received health care in India, quickly spread to Canada and other Western countries.
Adult Hospitals - Paediatric Hospitals - Overall
Source: Canadian Antimicrobial Resistance Surveillance System
"It needs to be tackled globally, because antimicrobial resistance cannot be contained within the geographical boundaries of countries," says Dr. Ramesh Agarwal, a neonatologist at All India Institute of Medical Sciences.
The decision to name the enzyme after the Indian capital outraged the country's government, which denied it had originated on the subcontinent.
But the incident was a "blessing in disguise," as it spurred the government to treat antimicrobial resistance seriously and start to act, says Dr. Chand Wattal, chairman of the microbiology department at Sir Ganga Ram Hospital.
"It just may not matter whether you have an antibiotic or not, because none are going to work."
Chairman of the microbiology department at Sir Ganga Ram Hospital Dr. Chand Wattal
The need to preserve antibiotic treatment is acute because otherwise "medical miracles" that are now taken for granted — including hip and knee replacements and liver transplants — could become impossible, he warns.
The risk of infection killing the patient would simply be too high. And the clock is ticking.
"I used to say in another 10 years. But now, I'm so afraid that I will say in another five years, if we are not discreet and we are indiscriminately using antibiotics," says Wattal.
"It just may not matter whether you have an antibiotic or not, because none are going to work."